Testing the Hearing
There are three stages to testing the hearing and all are important.
Audiograms can be wrong.
1 Clinical assessment of the degree of deafness.
2 Tuning fork tests.
3 Audiometry.
CLINICAL ASSESSMENT OF THE DEGREE
OF DEAFNESS
By talking to the patient, the examiner quickly appreciates how well a
patient can hear and this assessment continues throughout the interview.
A more formal assessment is then made by asking the patient to repeat
words spoken by the examiner at different intensities and distances in each
ear in turn. The result is recorded as, for example, whispered voice (WV)
at 150 cm in a patient with slight deafness, or conversational voice (CV) at
15 cm in a deafer individual.
If profound unilateral deafness is suspected, the good ear should be
masked with a Barany noise box and the deaf ear tested by shouting into it.
The limitations of voice and whisper tests must be borne in mind; they
are approximations but with practice can be a good guide to the level of
hearing and will confirm the audiometric findings.
TUNING FORK TESTS
Before considering tuning fork tests it is necessary to have a basic concept
of classification of deafness. Almost every form of deafness (and there are
many) may be classified under one of these headings:
• conductive deafness;
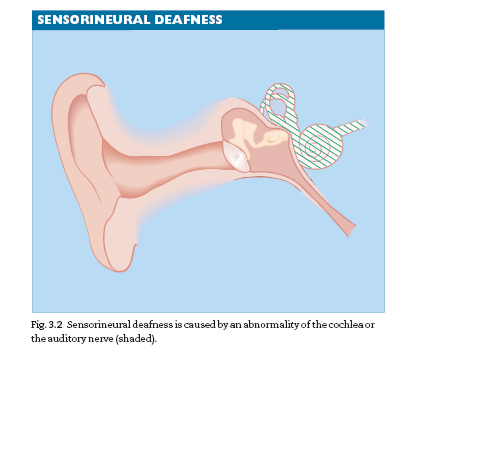
• sensorineural deafness;
• mixed conductive and sensorineural deafness.
Conductive deafness (Fig. 3.1)
Conductive deafness results from mechanical attenuation of the sound
waves in the outer or middle ear, preventing sound energy from reachingplaced firmly on the mastoid process and the patient is asked to state
whether it is heard better by BC or AC.
Interpretation of Rinne’s test
If AC>BC–called Rinne positive–the middle and outer ears are functioning
normally.
If BC>AC–called Rinne negative–there is defective function of the outer
or middle ear.
Rinne’s test tells you little or nothing about cochlear function. It is a test of
middle-ear function.
WEBER’S TEST
This test is useful in determining the type of deafness a patient may have
and in deciding which ear has the better-functioning cochlea. The base of
a vibrating tuning fork is held on the vertex of the head and the patient
is asked whether the sound is heard centrally or is referred to one or
other ear.
In conductive deafness the sound is heard in the deafer ear.
In sensorineural deafness the sound is heard in the better-hearing ear
SPEECH AUDIOMETRY
Speech audiometry is employed to measure the ability of each ear to discriminate
the spoken word at different intensities. A recorded word list is
supplied to the patient through the audiometer at increasing loudness
levels, and the score is plotted on a graph. In some disorders, the intelligibility
of speech may fall off above a certain intensity level. It usually
implies the presence of loudness recruitment—an abnormal growth of loudness
perception. Above a critical threshold, sounds are suddenly perceived
as having become excessively loud.This is indicative of cochlear disorder.
IMPEDANCE TYMPANOMETRY
Impedance tympanometry measures not hearing but, indirectly, the compliance
of the middle-ear structures. A pure tone signal of known intensity
is fed into the external auditory canal and a microphone in the ear probe
measures reflected sound levels.Thus, the sound admitted to the ear can be
measured. Most sound is absorbed when the compliance is maximal, and, by
altering the pressure in the external canal, a measure can be made of thecompliance at different pressures. Impedance testing is widely used as a
screening method for otitis media with effusion (OME) in children. If there
is fluid in the middle ear, the compliance curve is flattened.
ELECTRIC RESPONSE AUDIOMETRY
Electric response audiometry is a collective term for various investigations
whereby action potentials at various points within the long and complex
auditory pathway can be recorded. The action potential (AP) is evoked by
a sound stimulus applied to the ear either through headphones or free
field, and the resulting AP is collected in a computer store. Although each
AP is tiny, it occurs at the same time interval after the stimulus (usually a
click of very short duration) and so a train of stimuli will produce an easily
detectable response, while the averaging ability of the computer will
average out the more random electrical activity, such as the EEG. By making
the computer look at different time windows, responses at various sites
in the auditory pathway can be investigated. As the response travels from
the cochlea to the auditory cortex, the latency increases from about1-4 to 300 ms.


