Complications of Middle-Ear Infection
Acute mastoiditis
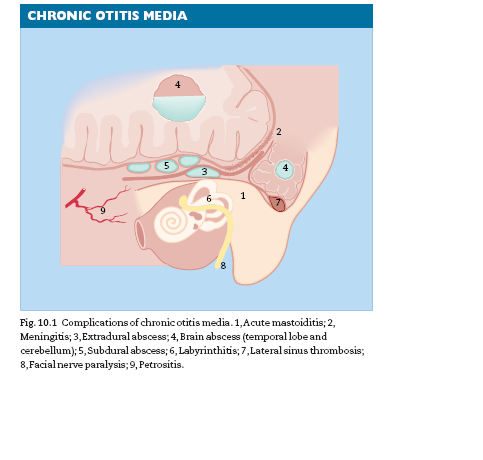
Acute mastoiditis is the result of extension of acute otitis media into the
mastoid air cells with suppuration and bone necrosis. Common in the
preantibiotic era, it is now rare in theWestern world (Fig. 10.1).
SYMPTOMS
1 Pain—persistent and throbbing.
2 Otorrhoea—usually creamy and profuse.
3 Increasing deafness.
SIGNS
1 Pyrexia.
2 General state—the patient is obviously ill.
3 Tenderness is marked over the mastoid antrum.
4 Swelling in the postauricular region, with obliteration of the sulcus.The
pinna is pushed down and forward (Fig. 10.2).
5 Sagging of the meatal roof or posterior wall.
6 The tympanic membrane is either perforated and the ear discharging,
or it is red and bulging.
If the tympanic membrane is normal, the patient does not have acute
mastoiditis.
INVESTIGATIONS
1 White blood count—raised neutrophil count.
2 CT scanning shows opacity and air cell coalescence.
OCCASIONAL FEATURES OF ACUTE MASTOIDITIS
1 Subperiosteal abscess over the mastoid process.
2 Bezold’s abscess—pus breaks through the mastoid tip and forms an
abscess in the neck.
3 Zygomatic mastoiditis—results in swelling over the zygoma.
TREATMENT
When the diagnosis of acute mastoiditis has been made, do not delay.The
patient should be admitted to hospital.
1 Antibiotics should be administered intravenously (i.v).The choice of antibiotic,
as always, depends on the sensitivity of the organism. If the organism
is not known and there is no pus to culture, start amoxycillin and
metronidazole immediately.
2 Cortical mastoidectomy. If there is a subperiosteal abscess or if the response
to antibiotics is not rapid and complete, cortical mastoidectomy
must be performed.The mastoid is exposed by a postaural incision and the
cortex is removed by drilling. All mastoid air cells are then opened, removing
pus and granulations. The incision is closed with drainage. The object
of this operation is to drain the mastoid antrum and air cells but leave the
middle ear, the ossicles and the external meatus untouched.
Meningitis
CLINICAL FEATURES
1 The patient is unwell.
2 Pyrexia—may only be slight.
3 Neck rigidity.
4 Positive Kernig’s sign.
5 Photophobia.
6 Cerebrospinal fluid (CSF)—lumbar puncture essential unless there is
raised intracranial pressure (q.v).
(a) Often cloudy.
(b) Pressure raised.
(c) White cells raised.
(d) Protein raised.
(e) Chloride lowered.
(f) Glucose lowered.
(g) Organisms present on culture and Gram stain.
TREATMENT
1 Do not give antibiotic until CSF has been obtained for culture and confirmation
of diagnosis.Then start penicillin parenterally and intrathecally.
2 Mastoidectomy is necessary if meningitis results from mastoiditis and
should not be delayed.The type of operation will be dictated by the extent
and nature of the ear disease.
Extradural abscess
An abscess formed by direct extension either above the tegmen or around
the lateral sinus (perisinus abscess).
The features of mastoiditis are present and often accentuated. Severe
pain is common.The condition may only be recognized at operation.
In addition to antibiotics, mastoid surgery is essential to treat the underlying
ear disease and drain the abscess.
Brain abscess
Otogenic brain abscess may occur in the cerebellum or in the temporal
lobe of the cerebrum.The two routes by which infection reaches the brain
are by direct spread via bone and meninges or via blood vessels, i.e.
thrombophlebitis.
A brain abscess may develop with great speed or may develop more
gradually over a period of months.The effects are produced by:
1 systemic effects of infection, i.e. malaise, pyrexia—which may be absent;
2 raised intracranial pressure, i.e. headache, drowsiness, confusion, impaired
consciousness, papilloedema;
3 localizing signs.
TEMPORAL LOBE ABSCESS
Localizing signs (Fig. 10.3):
1 dysphasia—more common with left-sided abscesses;
2 contralateral upper quadrantic homonymous hemianopia;
3 paralysis—contralateral face and arm, rarely leg;
4 hallucinations of taste and smell.
CEREBELLAR ABSCESS
Localizing signs:
1 neck stiffness;
2 weakness and loss of tone on same side;
3 ataxia—falling to same side;
4 intention tremor with past-pointing;
5 dysdiadokokinesis;
6 nystagmus—coarse and slow;
7 vertigo—sometimes.
DIAGNOSIS OF INTRACRANIAL SEPSIS:
1 Any patient with chronic ear disease who develops pain or headache
should be suspected of having intracranial extension.
2 Any patient who has otogenic meningitis, labyrinthitis or lateral sinus
thrombosis may also have a brain abscess.
3 Lumbar puncture may be dangerous owing to pressure coning.
4 Neurosurgical advice should be sought at an early stage if intracranial
suppuration is suspected.
5 Confirmation and localization of the abscess will require further
investigation.
Computerized tomography (CT) scanning will demonstrate intracranial
abscesses reliably and should always be performed when it is suspected.
Magnetic resonance (MR) imaging shows soft-tissue lesions with more detail
than CT but gives no bone detail. If in doubt what to do, discuss the problem with a radiologist.
TREATMENT
It is the brain abscess that will kill the patient, and it is this that must take surgical
priority.The abscess should be drained through a burr hole, or excised
via a craniotomy and then, if the patient’s condition permits, mastoidectomy
should be performed under the same anaesthetic. After pus has been
obtained for culture, aggressive therapy with antibiotics is essential, to be
amended as necessary when the sensitivity is known.
PROGNOSIS
The prognosis of brain abscess has improved with the use of antibiotics and
modern diagnostic methods but still carries a high mortality; the outlook is
better for cerebral abscesses than cerebellar, in which the mortality rate
may be 70%. Left untreated, death from brain abscess occurs from pressure
coning, rupture into a ventricle or spreading encephalitis.
Subdural abscess
Subdural abscess more commonly occurs in the frontal region from
sinusitis, but may result from ear disease. Focal epilepsy may develop from
cortical damage.The prognosis is poor.
Labyrinthitis
Infection may reach the labyrinth by erosion of a fistula by cholesteatoma. It
may rarely arise in acute otitis media.
CLINICAL FEATURES
1 Vertigo may be mild in serous labyrinthitis or overwhelming in purulent
labyrinthitis.
2 Nausea and vomiting.
3 Nystagmus towards the opposite side.
4 There may be a positive fistula test—pressure on the tragus causes
vertigo or eye deviation by inducing movement of the perilymph.
5 There will be profound sensorineural deafness in purulent labyrinthitis.
TREATMENT
1 Antibiotics.
2 Mastoidectomy for chronic ear disease.
3 Occasionally, labyrinthine drainage.
Lateral sinus thrombosis
A perisinus abscess from mastoiditis causes thrombosis of the lateral sinus
and ascending cortical thrombo-phlebitis. Septic emboli are given off and
metastatic abscesses may occur. The prognosis is poor but improved by
early diagnosis and treatment.
CLINICAL FEATURES
1 Swinging pyrexia—up to 40°C.
2 Rigors.
3 Polymorph leucocytosis.
4 Positive Tobey–Ayer test—sometimes. Compression of contralateral
internal jugular vein Æ rise in CSF pressure. Compression of ipsilateral
internal jugular vein Æno rise.
5 Meningeal signs—sometimes.
6 Positive blood cultures, especially if taken during a rigor.
7 Papilloedema—sometimes.
8 Metastatic abscesses—prognosis poor.
9 Cortical signs—facial weakness, hemiparesis.
TREATMENT
1 Antibiotics.
2 Mastoidectomy with wide exposure of the lateral sinus and even
removal of infected thrombus.
Facial paralysis
Facial paralysis can result from both acute and chronic otitis media.
1 Acute otitis media—especially in children and especially if the facial
nerve canal in the middle ear is dehiscent. It is, however, uncommon.
2 Chronic otitis media—cholesteatoma may erode the bone around the
horizontal and vertical parts of the facial nerve, and infection and granulations
cause facial paralysis.
In the early stages, the patient will complain of dribbling from the corner of
the mouth. Clinical examination confirms the diagnosis—it may be difficult
to detect if the weakness is minimal.
TREATMENT
If due to acute otitis media, a full recovery with antibiotic therapy is to be
expected.
If due to CSOM, mastoidectomy is mandatory, with clearance of disease
from around the facial nerve.
Remember—a facial palsy occurring in the presence of chronic ear disease is
not Bell’s palsy and active treatment is needed if the palsy is not to become
permanent. Do not give steroids.
Petrositis
Very rarely, infection may spread to the petrous apex and involve the VIth
cranial nerve.
CLINICAL FEATURES (GRADENIGO’S SYNDROME):
1 Diplopia from lateral rectus palsy.
2 Trigeminal pain.
3 Evidence of middle-ear infection.
TREATMENT
1 Antibiotics.
2 Mastoidectomy with drainage of the apical cells.


