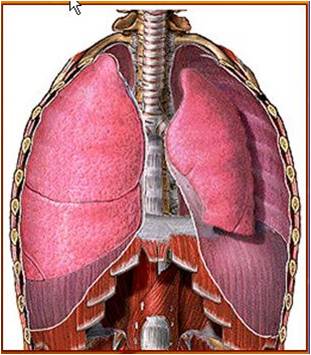
WEEK 25-30:Diseases of Lungs
Diagnosis and treatment of most respiratory disorders
depend heavily on understanding the basic
physiologic principles of respiration and gas
exchange. Some respiratory diseases result from
inadequate ventilation. Others result from abnormalities
of diffusion through the pulmonary membrane
or abnormal blood transport of gases
between the lungs and tissues. Therapy is often
entirely different for these diseases, so it is no longer satisfactory simply to make
a diagnosis of “respiratory insufficiency.”Chronic Pulmonary Emphysema
The term pulmonary emphysema literally means
excess air in the lungs. However, this term is usuallyused to describe complex obstructive and destructive
process of the lungs caused by many years of smoking.
It results from the following major pathophysiologic
changes in the lungs:
1. Chronic infection, caused by inhaling smoke or
other substances that irritate the bronchi and
bronchioles. The chronic infection seriously
deranges the normal protective mechanisms of the
airways, including partial paralysis of the cilia of
the respiratory epithelium, an effect caused by
nicotine. As a result, mucus cannot be moved
easily out of the passageways.Also, stimulation
of excess mucus secretion occurs, which further
exacerbates the condition. Too, inhibition of the
alveolar macrophages occurs, so that they become
less effective in combating infection.
2. The infection, excess mucus, and inflammatory
edema of the bronchiolar epithelium together
cause chronic obstruction of many of the smaller
airways.
3. The obstruction of the airways makes it especially
difficult to expire, thus causing entrapment of
air in the alveoli and overstretching them. This,
combined with the lung infection, causes marked
destruction of as much as 50 to 80 per cent of the
alveolar walls
.Pneumonia
The term pneumonia includes any inflammatory conditionA common type of pneumonia is bacterial pneumonia,
caused most frequently by pneumococci.
This disease begins with infection in the alveoli; the
pulmonary membrane becomes inflamed and highly
porous so that fluid and even red and white blood cellsleak out of the blood into the alveoli.Thus, the infected
alveoli become progressively filled with fluid and cells,
and the infection spreads by extension of bacteria or
virus from alveolus to alveolus. Eventually, large areas
of the lungs, sometimes whole lobes or even a whole
lung, become “consolidated,” which means that they
are filled with fluid and cellular debris.
In pneumonia, the gas exchange functions of the
lungs change in different stages of the disease. In early
stages, the pneumonia process might well be localized
to only one lung, with alveolar ventilation reduced
while blood flow through the lung continues normally.
This results in two major pulmonary abnormalities: (1)
reduction in the total available surface area of the respiratory
membrane and (2) decreased ventilationperfusion
ratio. Both these effects cause hypoxemia
(low blood oxygen) and hypercapnia (high blood
carbon dioxide).
of the lung in which some or all of the alveoli
are filled with fluid and blood cells,


