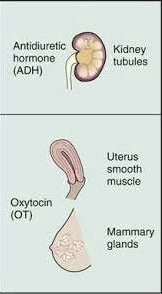
POSTERIOR PITUITARY HORMONES
The posterior pituitary gland secrets ADH and oxytocin hormones which are synthesized in the hypothalamus and are released into the neurohypophyseal capillaries which surround the gland. Antidiuretic hormone (ADH) is synthesized in the supraoptic nuclei of the hypothalamus while oxytocin is synthesized in the paraventricular nuclei of the hypothalamus.
Antidiuretic Hormone (ADH)
ADH, also known as vasopressin, acts as a water preserving hormone. ADH is released into the blood circulation to vasoconstrict and reabsorbs water from the collecting duct in the kidney to maintain equilibrium intracellularly and extracellularly. In the hypothalamus, there are two regulating receptors that sense water depletion and hyperosmolar concentration, the subfornical organ, and organum vasculosum. This particular area of the nervous system does not have an intact blood-brain barrier. Therefore, blood products can come into contact with the structures with ease and eventually signal the hypothalamus for ADH secretion. A small concentration is enough to generate water conservation in the renal tubules. The renal tubules are broken down into segments known as the proximal, descending, ascending, distal, and collecting duct. The collecting duct is a highly diluted, ADH dependent structure in the kidney. The cells in the collecting duct have a 7 pass receptor on the basolateral side where ADH can bind itself. The signal unleashes a power generating cascade known as cAMP. The Gs protein stimulates adenylyl cyclase, which converts ATP into cAMP. High concentration of cAMP will phosphorylate protein kinase A, opening water channels to allow passage from the luminal side to the basolateral side. The channels are gated vesicles known as aquaporins. The amount of water absorbed from the collecting duct is dependent on the amount of fluid loss.
Oxytocin
Oxytocin is a polypeptide hormone that is produced in the paraventricular nuclei for storage and release from the pituitary gland. It is commonly excreted in females during the birthing process. It functions to allow the uterus to contract, release milk from the breast and is present during ejaculation in males.
Oxytocin: Uterus
When the fetus reaches an appropriate size, it stretches the uterine muscle lining, transmitting signals to the hypothalamus which generates and releases oxytocin into the systemic circulation. The hormone binds to the myometrial layer of the uterus where the smooth muscle is present. Once oxytocin attaches to the extracellular receptor, it activates the Gq protein, which then activates another cell membrane protein called Phospholipase C. PLC will break down phosphoinositol diphosphate in two components, diacylglycerol (DAG) and Inositol triphosphate (IP3). IP3 will push calcium from the sarcoplasmic reticulum while DAG activates protein kinase C. This protein will phosphorylate proteins on the cell membrane to specifically allow calcium entry from extracellular space. An increase in intracellular calcium will generate enough energy to cause contraction of the uterus advancing the fetus into the vagina for delivery.
Oxytocin: Lactation
The regulation of lactation is similar to uterine contraction where an external source stimulates the production of oxytocin by the hypothalamus. During lactation, the newborn, by means of “suckling”, will transmit a signal to the central nervous system. This process is known as the “milk letdown reflex.” Once oxytocin binds to myoepithelial cell receptors in the breast it will undergo the same Gq cascade as uterine contraction, ejecting milk forward into the baby’s oral cavity.
By the end of this lesson, students should learn about
- Physiological functions of antidiuretic hormone
- Regulation of antidiuretic hormone production
- Functions of oxytocin hormone


